Lab-Grown Liver Tissue: A Breakthrough for Hemophilia and Organ Transplants
Scientists have achieved a significant milestone in regenerative medicine by creating lab-grown liver tissue capable of forming its own blood vessels. This groundbreaking development offers renewed hope for individuals suffering from hemophilia and holds immense potential for future organ transplantation.
The Promise for Hemophilia Patients
Hemophilia, a genetic disorder that impairs the body’s ability to control blood clotting, often requires frequent infusions of clotting factors. Lab-grown liver tissue could provide a more sustainable solution. Here’s why:
- Natural Clotting Factor Production: The engineered tissue is designed to produce essential clotting factors, potentially reducing or eliminating the need for external infusions.
- Reduced Bleeding Episodes: By restoring the body’s natural clotting mechanisms, this technology aims to significantly decrease the frequency and severity of bleeding episodes in hemophilia patients.
- Improved Quality of Life: A successful implementation of this technology could dramatically improve the quality of life for individuals living with hemophilia, allowing them to lead more active and fulfilling lives.
Implications for Organ Transplantation
Beyond hemophilia, this research has far-reaching implications for organ transplantation:
- Addressing Organ Shortages: The ability to grow functional liver tissue in the lab could help alleviate the critical shortage of donor organs, saving countless lives.
- Personalized Medicine: Lab-grown tissue can be tailored to the specific needs of each patient, minimizing the risk of rejection and improving transplant outcomes.
- Drug Testing and Research: Engineered liver tissue provides a valuable platform for drug testing and disease modeling, accelerating the development of new therapies and treatments.
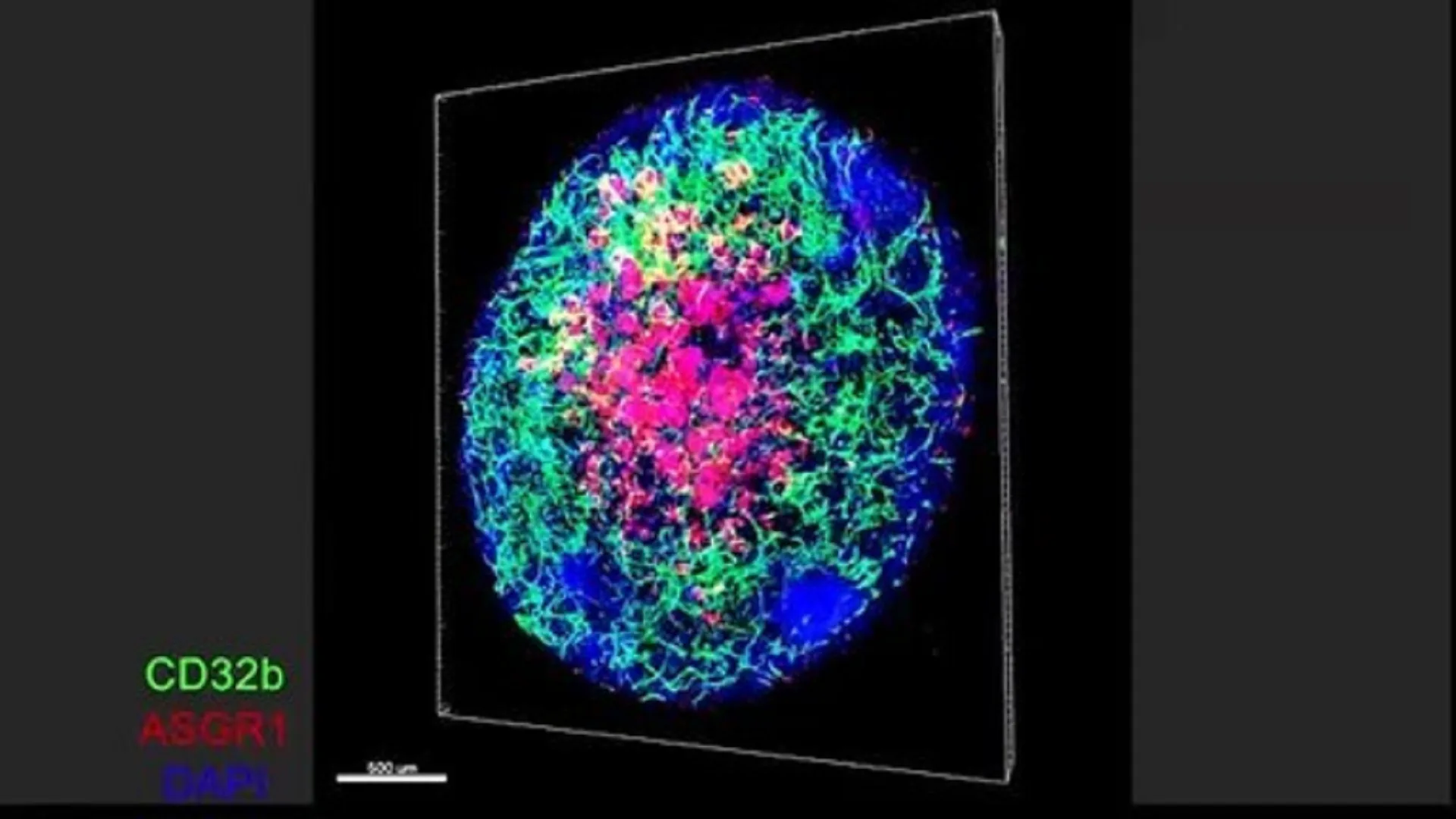
How the Breakthrough Was Achieved
The key to this breakthrough lies in the tissue’s ability to self-assemble blood vessels. This vascularization is crucial for:
- Nutrient Delivery: Blood vessels ensure that the engineered tissue receives the necessary nutrients and oxygen to survive and function.
- Waste Removal: They also facilitate the removal of waste products, preventing tissue damage and promoting long-term viability.
- Integration with Host Tissue: The formation of blood vessels allows the lab-grown tissue to integrate seamlessly with the recipient’s own circulatory system, enhancing its functionality.
Challenges and Future Directions
While this achievement represents a major step forward, challenges remain:
- Scaling Up Production: Researchers need to develop methods for producing large quantities of functional liver tissue.
- Long-Term Viability: Ensuring the long-term survival and functionality of the engineered tissue in vivo is crucial.
- Clinical Trials: Rigorous clinical trials are necessary to evaluate the safety and efficacy of this technology in human patients.
Final Overview
The development of lab-grown liver tissue with self-forming blood vessels represents a significant advancement in regenerative medicine. With continued research and development, this technology holds immense promise for treating hemophilia, addressing organ shortages, and revolutionizing healthcare.


+ There are no comments
Add yours